Healthcare workers open up about their experiences with COVID-19
Published 6:07 pm Tuesday, May 5, 2020
|
Getting your Trinity Audio player ready...
|
By SCOTT MIMS / Staff Writer
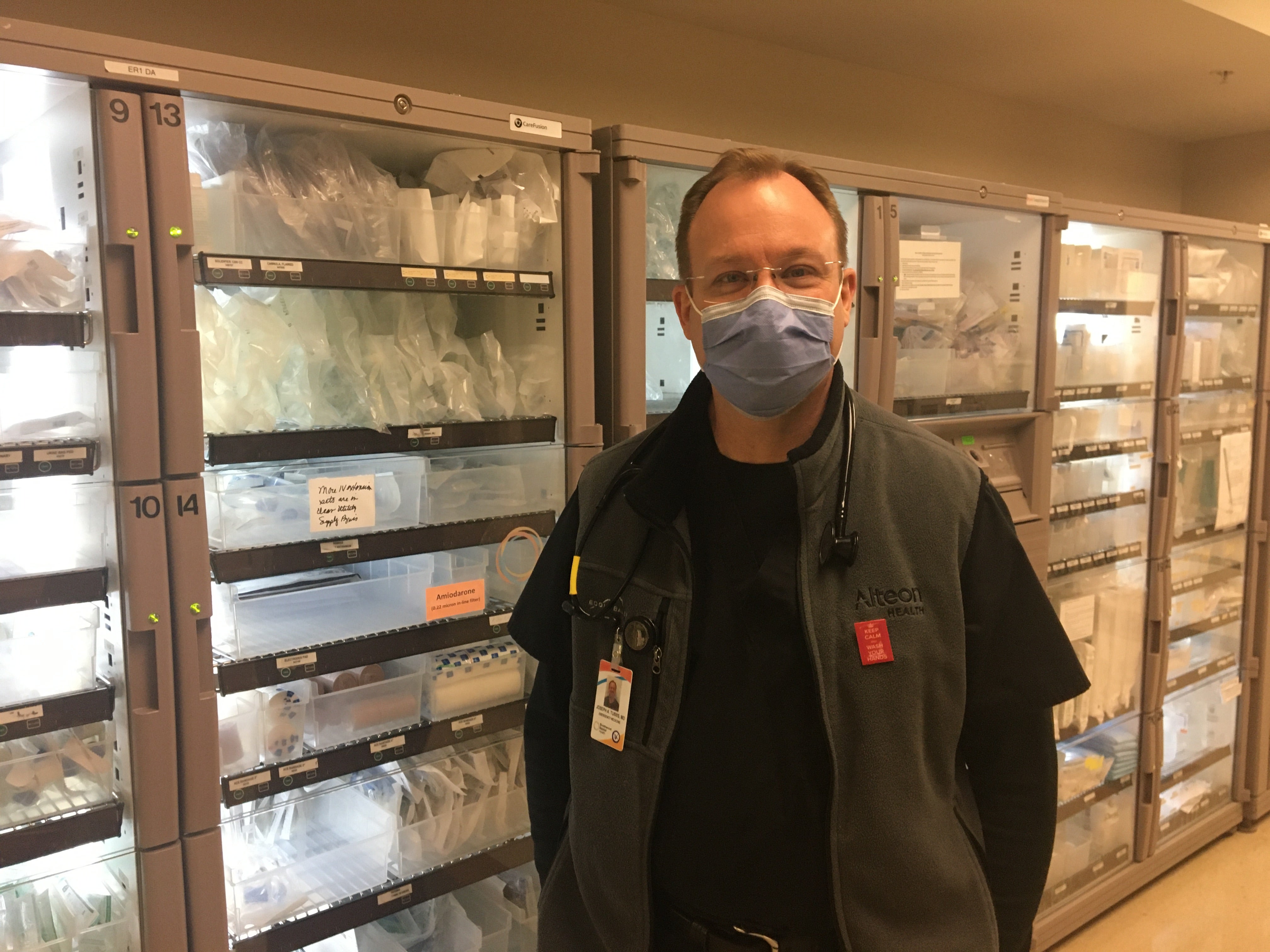
ALABASTER — Dr. Joseph A. Tubbs’ first encounter with COVID-19 was a chilling one.
Tubbs saw a patient at Shelby Baptist Medical Center for an unrelated complaint. The woman showed no signs of fever, cough or other upper respiratory symptoms. He spoke with her about test results and said he wanted to keep her in the hospital overnight just for precautions, and she agreed.
“I remember her laughing with her husband about missing some family event because she was going to spend the night the hospital,” said Tubbs, adding that the patient went home the next day fine.
“She came back four days later in respiratory failure and was immediately placed on life support while still in the emergency department, admitted to the hospital and ultimately passed away,” Tubbs said. “The dramatic change that occurred in only four days from an adult full of life, joking with her husband about daily life’s minutia to a critically unwell person who needed to be placed on life support within 15 minutes of arrival to the ED and ultimately succumbed to her illness gave me a healthy respect for this virus. And ultimately the experience served to foreshadow the seriousness of this illness in certain individuals.”
Tubbs, chairman of the Department of Emergency Medicine at Shelby Baptist, is one of many on the front lines to witness the unpredictability of COVID-19. And even though healthcare workers have always followed thorough sanitization procedures, the novel coronavirus has changed even the way they approach things—at least from an awareness perspective.
“We’ve always been conscientious about hand hygiene in the Emergency Department (ED) given the nature of what we do; however, it seems like everything has been increased as far as our overall awareness,” Tubbs said. “Before all of this started, I never consciously thought of my overall distance from a patient or family members in the room. Now I find myself positioning in the room so that we all are properly spaced. The additional time it takes to don and doff the different levels of PPE requirements has certainly made us less efficient, but it’s an acceptable trade-off because it makes everybody safer.”
Tubbs said a mere six weeks ago it would have seemed unfathomable to not physically examine a patient using one’s hands, but now, if a patient has a straightforward complaint such as a urinary tract infection, the exam consists of visually looking at the patients and speaking with them.
Personally, Tubbs refuses to even enter an exam room until asking whether a patient has had possible COVID-19 symptoms such as coughing, fever, body aches or has been exposed to the virus—and getting an answer from the patient.
For RN Ashley Terrell, the biggest change has been having to wear PPE constantly—that and the unprecedented isolation of COVID-19 patients she has witnessed.
“The fact that loved ones cannot be with these patients during their last moments on this earth is sad. It is something I never thought we would have to deal with as healthcare providers,” Terrell said.
Still, Tubbs said he felt Shelby County has been “relatively well cocooned” from COVID-19; he estimated that Shelby Baptist is seeing an average of less than 10 patients a day suspected to have the virus. And the majority of them go home with instructions to self-quarantine until their symptoms fade—something even Tubbs is having to get used to.
“From a personal perspective it is a little strange diagnosing a person with a disease, and then telling them simply to go home, and stay home,” he said. “We’ve become so accustomed to modern western medicine of having a prescription or treatment regimen for most everything that this just feels different.”
For the patients who are harder hit, such as the woman from Tubbs’ first encounter, however, it’s a different story.
Terrell said patients who have COVID-19 are very sick.
“It is a kind of sick we have never seen before,” she said.
But perhaps the most unexpected part of the crisis has nothing to do with the virus itself or even the statistics—it seems to be the great outpouring of support from the general public for those like Tubbs and Terrell.
Tubbs said that just knowing someone is keeping him in their thoughts and prayers for a job he has done for nearly 20 years has been “surprising.”
“It feels like we have been placed in a spotlight in a positive way,” he said. “The people that are around us every day—hospital administration, fellow physicians, nurses, clerks, techs, all of the support staff which help us on the front lines to do our job—have been highlighted.”
Indeed, healthcare workers face a fear many people share but to a much greater degree—that of the possibility of bringing coronavirus home to their family. This occurs for the obvious reason that they know without a doubt they have been around the virus.
“I know that myself and many other nurses wonder, ‘Have I done enough to protect myself throughout my 12-hour shift?’ Terrell said. “I’m always trying to make sure that I do not spread it to my husband or children.”
At the same time, nurses and doctors must provide some reassurance to COVID-19 patients as well as other patients who are nervous about being in a hospital during the pandemic.
Tubbs said he has even had patients to apologize for coming to the ED after an accident that resulted in a broken bone or laceration.
“What I tell them is, ‘This is what we’re here for; this is what we do.’ I try to reassure them that they’re in a safe environment. They are in a cleaner (safer) environment than probably the car they drove to the ED. I try to reassure them that we will do everything within our power to minimize the amount of time that they spend in the hospital,” he said.
Terrell said suspected COVID-19 patients are scared, and they constantly read about symptoms, which seems to feed their cycle of fear.
She said that while people should respect the virus, they should not be in a constant state of fear because fear leads to panic.
“We reassure the patients by letting them know that we are here for them, to help them in any way we can and that we will do what it takes to keep them safe and help get them better,” she said.
When asked what advice he would give the community during the pandemic, Tubbs said just to know that every little bit helps when it comes to social distancing, self-quarantining for symptomatic people, and a heightened sense of awareness.
“I believe when you look at these practices at a community-wide level, they work,” he said.
Tubbs expressed thanks to the hospital, administration, community, coworkers, friends and family who have supported workers like Terrell and himself.
Both indicated that they believe the community, state and nation will ultimately outlast the virus.
“This is what we do,” Tubbs said. “We did it last year, we did it last week and we’re going to be here tomorrow and the year after that. I truly believe that we will beat this.”